Reading Time: 25-30 minutes
Author: NStarX Engineering team focused on Healthcare Provider domain. This blog post presents analysis and synthesis based on publicly available research, industry reports, and news sources. All statistics and claims are supported by the cited references. The views expressed represent an independent assessment of the EHR landscape and do not constitute medical, legal, or financial advice. Healthcare organizations should conduct their own due diligence when evaluating technology investments.
Introduction
The American healthcare system stands at a crossroads. While electronic health records promised to revolutionize healthcare delivery, reduce medical errors, and improve patient outcomes, the reality has been far more complex. Today, as we examine the $12.87 billion U.S. EHR market, we find a landscape characterized by both tremendous progress and significant challenges—challenges that artificial intelligence, particularly through innovative approaches like federated learning, may finally be positioned to address.
Section 1: Understanding the US EHR Market and Ecosystem
What is an Electronic Health Record?
An Electronic Health Record (EHR) is a comprehensive digital version of a patient’s paper chart, containing a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results. Unlike simple digitized records, EHRs are designed to be shared across different healthcare settings—from primary care physicians to specialists, from hospitals to laboratories—creating a coordinated approach to patient care.
The Size and Scope of the US EHR Market
The US EHR market has experienced explosive growth over the past decade. As of 2024, the market was valued at approximately $12.87 billion and is projected to reach $43.36 billion by 2030, growing at a CAGR of 2.55-4.54% depending on the segment. This growth is fueled by government initiatives, technological advancement, and an increasing demand for centralized healthcare data to improve patient outcomes while reducing costs.
The United States accounts for over 38% of the global EHR market, driven by high penetration rates across healthcare facilities:
- Hospital Adoption: As of 2024, hospitals represent 52.94% of the EHR market share, with adoption rates reaching 81.2%, up from just 6.6% in the early 2000s.
- Ambulatory Care: The ambulatory EHR segment is growing fastest, valued at $6.75 billion in 2025 and expected to reach $8.96 billion by 2030.
- Specialty Segments: Different healthcare sectors utilize EHRs differently—from acute care (45.89% market share) to post-acute care facilities, rehabilitation centers, and mental health services.
Market Segmentation
The EHR ecosystem spans multiple dimensions:
By Deployment Model:
- Cloud & Web-Based Systems: 83.27% market share in 2024, preferred for scalability and lower infrastructure costs
- On-Premise Systems: Declining due to lack of interoperability, limited scalability, and high maintenance costs
By Type:
- Acute EHR Systems
- Ambulatory EHR Systems
- Post-Acute EHR Systems
By Business Model:
- Professional Services: 32.33% market share
- Licensing and Subscription Models
- Managed Services
By End User:
- Hospitals and Health Systems
- Physician Practices
- Long-term Care Facilities
- Specialty Clinics
The Lifecycle of an EHR System
The EHR lifecycle encompasses multiple stages, each critical to successful implementation and operation:
1. Planning and Selection (6-12 months)
- Needs assessment and stakeholder alignment
- Vendor evaluation and selection
- Budget allocation and ROI analysis
2. Implementation (12-24 months)
- System configuration and customization
- Data migration from legacy systems
- Integration with existing healthcare IT infrastructure
- Workflow redesign
3. Training and Go-Live (3-6 months)
- End-user training programs
- Phased or “big bang” deployment
- Immediate post-launch support
4. Optimization and Maintenance (Ongoing)
- Continuous system refinement
- Regular software updates
- Performance monitoring
- User feedback integration
5. Evolution and Expansion (Ongoing)
- Addition of new modules
- Integration with emerging technologies (AI, telehealth, wearables)
- Adaptation to regulatory changes
- Interoperability enhancements
Section 2: The Evolution of EHR Over the Last Decade (2015-2025)
Key Milestones in EHR Evolution
The past decade has been transformative for the EHR industry, shaped by legislation, technological advancement, and changing healthcare delivery models. NStarX has been fortunate to be part of this journey. NStarX engineering team played a pivotal role in building the OneEHR platform that was cloud native and meaningfully certified by HHS. The product is still one of the core offerings as part of AthenaHealth.
2009-2011: The HITECH Act Foundation The Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009, fundamentally changed the trajectory of healthcare IT. The government allocated $27 billion in Medicare and Medicaid incentive payments to drive EHR adoption through “meaningful use” criteria.
Meaningful Use Stage 1 (2011-2013): Data Capture and Sharing
- Focus on electronically capturing clinical data
- Requirements for e-prescribing
- Patient access to electronic health records
- Adoption rates climbed from 3.2% in 2008 to 14.2% by 2015
Meaningful Use Stage 2 (2014-2016): Advanced Clinical Processes
- Expanded data fields including images and family history
- Increased patient engagement through patient portals
- Electronic transmission of data to public health agencies
- By 2017, 86% of office-based physicians and 96% of non-federal acute care hospitals had adopted EHRs
Meaningful Use Stage 3 (2017): Improved Outcomes
- Continuous requirement to meet all program objectives
- Focus on interoperability and patient engagement
- Integration with population health management
- Penalties began for providers not demonstrating meaningful use (1% Medicare reduction in 2015, rising to 3% by 2017)
2016: The 21st Century Cures ActThis landmark legislation mandated stricter interoperability requirements and prohibited information blocking—the practice of knowingly interfering with the exchange or use of electronic health information.
2018: Promoting Interoperability ProgramCMS renamed Meaningful Use to the Promoting Interoperability program, shifting focus from adoption to interoperability and becoming part of the Medicare Merit-Based Incentive Payment System (MIPS).
2020-2021: COVID-19 Acceleration The pandemic dramatically accelerated EHR adoption and integration with telehealth platforms. Healthcare organizations were forced to rapidly digitize operations, leading to:
- Integration of telemedicine capabilities within EHR platforms
- Remote patient monitoring integration
- Enhanced patient portal usage
- Virtual care documentation workflows
2022-2024: AI Integration Begins Major EHR vendors began integrating artificial intelligence capabilities:
- Epic introduced predictive analytics for sepsis identification
- Oracle Health (formerly Cerner) launched cloud-based AI-powered EHR
- Microsoft’s Nuance DAX Copilot brought ambient clinical documentation
- Ambient AI scribe market reached $600 million in 2025
2025: The Agentic AI Era The industry entered a new phase with autonomous AI agents capable of:
- Automated clinical documentation
- Intelligent clinical decision support
- Predictive patient deterioration alerts
- Natural language query of EHR data
- Autonomous clinical coding
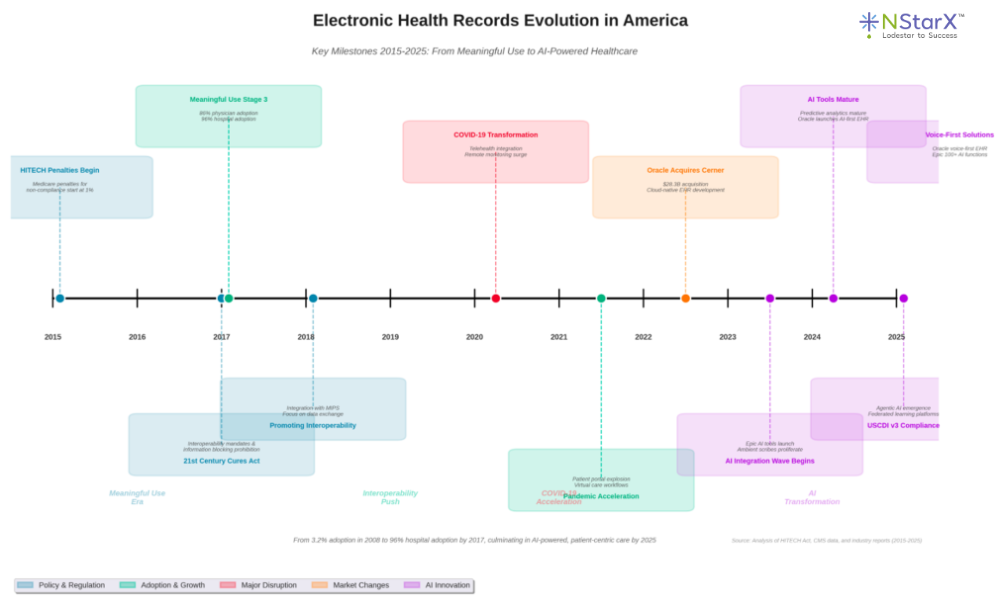
Visual Timeline: EHR Evolution 2015-2025
Figure 1: It shows the Electronic Health Record Evolution in the US over the last 10 years
Section 3: The Broken EHR System—Challenges and Dependencies
Despite significant progress, the current EHR ecosystem suffers from fundamental structural problems that impede its promise of seamless, patient-centered care.
The Interoperability Crisis
The most critical failure of modern EHRs is their inability to communicate effectively with each other. While government mandates have pushed vendors toward standard protocols like FHIR (Fast Healthcare Interoperability Resources), implementation remains inconsistent and often deliberately limited.
The Cost of Poor Interoperability Economists estimate that inadequate interoperability still costs the U.S. healthcare system billions annually through:
- Duplicate testing and procedures
- Delayed diagnoses
- Medication errors from incomplete information
- Administrative burden of manual data reconciliation
- Lost productivity in data retrieval
The Epic Monopoly Problem
Epic Systems Corporation has emerged as the dominant force in the EHR market, controlling the health records of up to 94% of Americans. While Epic’s market dominance speaks to its comprehensive product suite, it has created several problematic dynamics:
Market Control and Anti-Competitive Behavior Recent legal challenges have highlighted concerning practices:
- In 2025, Particle Health filed a federal antitrust lawsuit alleging Epic used its monopoly power to block competitors from the emerging payer platform market
- Epic was identified in a 2014 RAND report as a “single roadblock to interoperability”
- Critics argue Epic prioritizes data exchange between Epic clients while creating barriers for non-Epic systems
The Cost Burden Epic implementations are notoriously expensive:
- Licensing fees run into millions of dollars
- Customization and integration require specialized (and expensive) technical resources
- Ongoing maintenance and upgrade costs create long-term financial commitments
- Small and medium-sized providers often cannot afford Epic, creating a two-tier system
Vendor Lock-In Once organizations commit to Epic, switching costs become prohibitive:
- Years of patient data locked in proprietary formats
- Workflow dependencies on Epic-specific features
- Staff training investments
- Integration dependencies with other systems
Government Policy Dependencies
The EHR ecosystem remains heavily dependent on government regulation and incentive structures:
Meaningful Use Evolution: The transition from incentive-based to penalty-based compliance created financial pressure but didn’t necessarily improve usability or clinical outcomes.
TEFCA Implementation: The Trusted Exchange Framework and Common Agreement (TEFCA), effective January 2025, mandates national exchange specifications. However, implementation remains inconsistent and enforcement unclear.
USCDI Standards: The United States Core Data for Interoperability (USCDI), now in version 4, defines standardized data elements. Certified health IT developers must complete real-world testing by December 2025, but compliance varies.
The 21st Century Cures Act: While this legislation prohibited information blocking, enforcement has been limited:
- Penalties for blocking information can reach 5% Medicare payment cuts
- Potential removal from the Shared Savings Program
- Reputational harm, yet actual enforcement cases remain rare
Integration Challenges with Large Systems
Beyond Epic, the EHR landscape is dominated by a handful of large vendors, each with proprietary approaches:
Oracle Health (formerly Cerner)
- 21.7% market share in acute care
- Lost 74 hospitals and 17,232 beds in 2024
- Complex migration from Cerner to Oracle’s new cloud platform
- Integration challenges with Oracle’s broader enterprise systems
Athenahealth
- Cloud-native platform with percentage-of-collections pricing
- 277,000+ clinical integrations
- Strong in ambulatory care but limited in hospital settings
MEDITECH
- Strong legacy customer retention
- Enhanced technology for modern workflows
- Limited market growth compared to Epic
The CommonWell Problem: Many EHR vendors formed the CommonWell Health Alliance to create interoperability standards, but Epic notably refused to join, fragmenting data exchange efforts.
Technical and Workflow Problems
User Interface Challenges
- Information overload: clinicians see all patient data regardless of relevance
- Slow system response times
- Excessive clicks required for common tasks
- Poor navigation requiring multiple tabs and pages
- “Note bloat” from defensive documentation
Data Entry Burden
- Physicians spend 2 hours on EHR work for every 1 hour of direct patient care
- Documentation designed for billing rather than clinical care
- Redundant data entry across systems
- Copy-paste errors and outdated information propagation
Legacy System Integration
- Many organizations run multiple EHR systems from mergers and acquisitions
- UPMC, for example, is consolidating from nine different EHR systems
- Data migration challenges
- Inconsistent data formats
Compliance and Regulatory Complexity
HIPAA and Privacy Requirements
- Business associates must comply with strict privacy rules
- Breach notification requirements for incidents affecting 500+ patients
- Complex consent management
- State-specific privacy laws (like California’s CCPA)
Quality Reporting Mandates
- MIPS quality measures require extensive EHR configuration
- Clinical Quality Measures (CQMs) add documentation burden
- Value-based care metrics tied to EHR capabilities
Prior Authorization Challenges
- EHRs often lack real-time payer coverage information
- Manual prior authorization processes despite electronic capabilities
- Delayed care and administrative burden
Section 4: Impact on Patients and Healthcare Providers
The broken EHR system extracts a heavy toll on both those who use it and those it’s meant to serve.
Quantifiable Impact on Healthcare Providers
Physician Burnout Epidemic — The statistics are sobering:
- Nearly 75% of physicians identify the EHR as a source of burnout symptoms
- 27.2% of physicians using EHRs report one or more burnout symptoms, compared to 13.6% of non-EHR users
- Burnout prevalence reaches almost 50% in primary care
- Family physicians had the third-highest prevalence of health IT-related stress at 83.2%
Time Burden — Physicians report spending excessive time on EHR-related tasks:
- Up to 2 hours of EHR work for every 1 hour of face-to-face patient care
- Large amounts of time working on EHRs at home (“pajama time”)
- 70% of physicians report at least one measure of health IT-related stress
- EHR inbox messages correlate directly with burnout
Clinical Impact
- Reduced eye contact and connection with patients during encounters
- Compromised clinical decision-making from information overload
- Increased risk of medical errors from copy-paste documentation
- Reduced time for thoughtful patient interaction
Economic Consequences for Providers
- Physicians retiring early due to EHR burden
- Increased turnover in primary care
- Need to hire medical scribes (where affordable)
- Productivity loss from inefficient workflows
Real-World Examples of Provider Challenges
Case Study: Rhode Island Physician Survey A survey of nearly 1,800 physicians in Rhode Island found:
- Over 91% used an EHR
- Nearly 70% reported at least one measure of health IT-related stress
- Only 50% thought EHRs improved patient care or clinical workflow
- Less than 30% reported EHRs improve job satisfaction
- Despite benefits in billing (75% agreement) and communication (69% agreement), negatives outweighed positives
Case Study: Change Healthcare Ransomware Breach (2024) The ALPHV ransomware breach demonstrated the fragility of centralized healthcare data systems:
- Triggered revenue losses for 80% of U.S. physician practices
- Required a $22 million ransom payment
- Produced multi-week payment delays
- Exposed vulnerabilities in centralized data storage
Case Study: Epic Access Blocking According to Particle Health’s 2025 lawsuit, Epic allegedly blocked doctors’ access to records of more than 2,800 patients in a network of community oncology practices—demonstrating how vendor disputes can directly harm patient care.
Impact on Patients
- Fragmented Care Experience
- Patients must repeat medical history at each new provider
- Test results get lost between systems
- Medication lists become outdated across providers
- Care coordination failures lead to duplicate testing
- Safety Concerns
- Medication errors from incomplete allergy information
- Adverse drug interactions missed due to fragmented records
- Delayed diagnoses from unavailable prior imaging or test results
- Higher morbidity and mortality from care coordination failures
- Access and Engagement Challenges
- Inconsistent patient portal experiences across providers
- Difficulty obtaining complete medical records
- Limited ability to aggregate personal health data
- Digital divide excludes those without technical literacy
- Financial Burden
- Redundant testing due to unavailable records
- Delayed care from prior authorization bottlenecks
- Higher costs from preventable complications
- Out-of-pocket expenses for record retrieval
The Paradox of Progress
Despite EHRs achieving near-universal adoption, fundamental problems persist:
- More data is being captured than ever before, but it’s harder to find the right information
- Systems are more connected technically, but clinical information flow remains broken
- Billions have been invested, but provider satisfaction is at historic lows
- Patients have more access to their records, but understanding and using that information remains challenging
Section 5: The Landscape of AI Solutions Addressing EHR Challenges
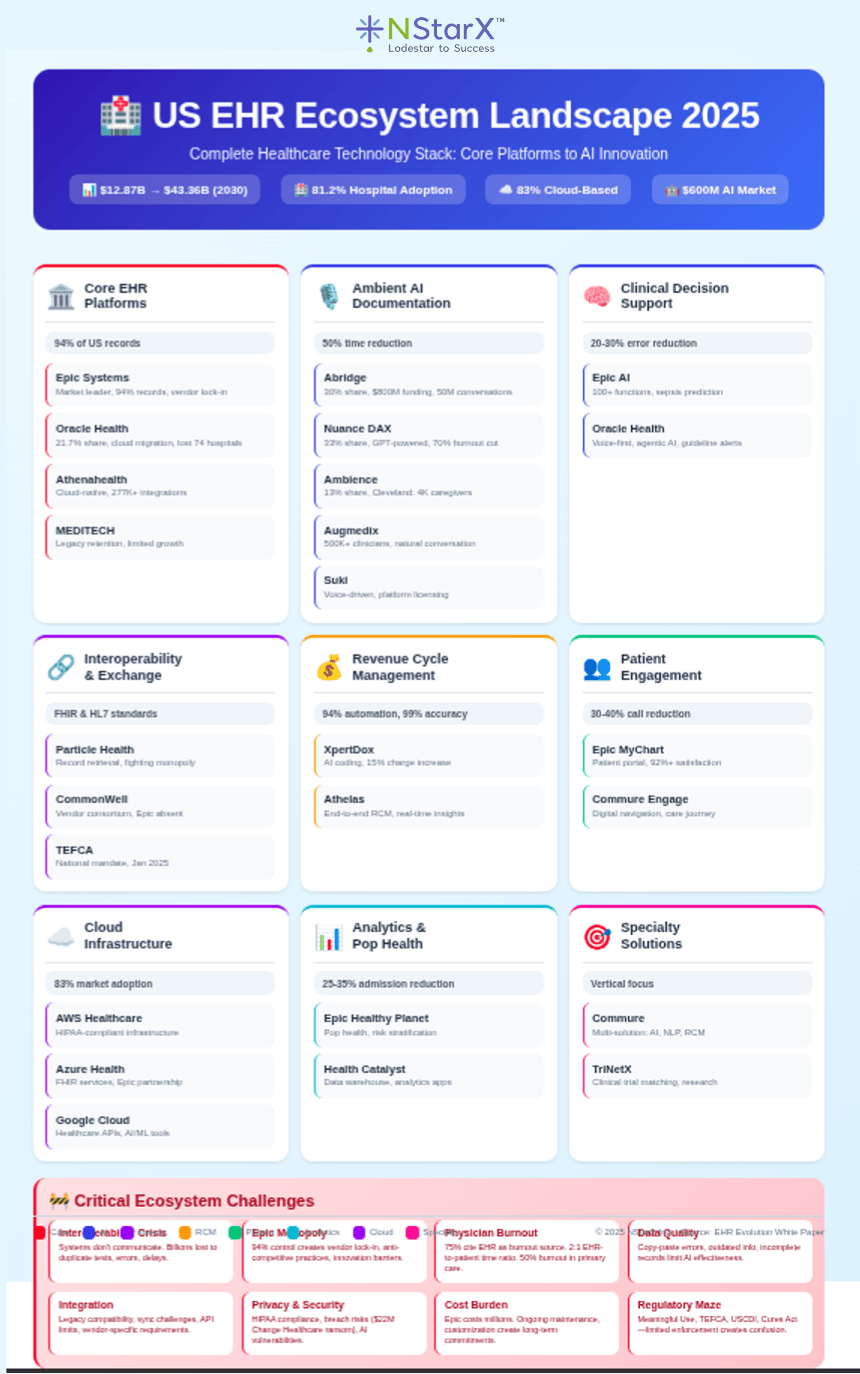
NStarX has put together an EHR landscape that is our observation. It may vary in the eyes of the domain expertise:
Figure 2: Landscape of the EHR functional Ecosystem
A new wave of artificial intelligence companies and capabilities is emerging to address the fundamental problems plaguing EHR systems. While these solutions show tremendous promise, they also face significant challenges in deployment, integration, and adoption.
The Ambient AI Revolution
Market Growth and Adoption Ambient scribes have become healthcare AI’s first breakout category:
- Generated $600 million in revenue in 2025, up 2.4x year-over-year
- Over 170-180 healthcare organizations using ambient AI as of 2025
- Two new unicorns emerged: Abridge (30% market share) and Ambience Healthcare (13% market share)
- Microsoft’s Nuance DAX Copilot maintains 33% market share
Key Players and Their Approaches
Abridge
- Raised $300 million in Series E (June 2025), bringing total funding to $800 million
- Launched Abridge Inside for Emergency Medicine
- Expanded to inpatient documentation and nursing workflows
- Partnerships with Epic, Mayo Clinic, and Wolters Kluwer
- Expected to support over 50 million medical conversations in 2025
Ambience Healthcare
- Focus on comprehensive clinical documentation automation
- Cleveland Clinic deployed across 4,000+ caregivers with reported success
- “One of the most successful technology launches” according to Cleveland Clinic CIO
Microsoft Nuance DAX Copilot
- Leverages GPT models for fine-tuning and customization
- Integration with major EHR platforms
- Up to 50% reduction in documentation time
- 70% reduction in burnout feelings reported in studies
Augmedix
- AI-powered ambient documentation capturing natural conversations
- Converts conversations into structured medical notes and data entries
- Supporting nearly half a million clinicians
- Data from millions of clinical interactions
Suki
- Voice-driven AI layer for clinical workflows
- Ambient documentation and voice-based form filling
- Licenses technology through Suki Platform for partners
- Combines speech recognition, LLMs, and medical context
Documented Impact
- Kaiser Permanente: Cut clinician documentation time by up to 2 hours per day; patient satisfaction scores above 92%
- Northeast Medical Specialists: Achieved near-perfect note accuracy, 30% reduction in documentation time with Epic-integrated solution
- Dignity Health physicians: Save up to 3 hours per day on charting, plus 4 additional hours on weekends
Clinical Decision Support and Predictive Analytics
Epic’s AI Capabilities
- Built over 100 AI functions within the EHR
- Sepsis identification and early warning systems
- Automated MyChart messaging
- Order prediction based on clinical context
- SlicerDicer Sidekick agent for data analysis
Oracle Health’s Next-Gen EHR
- Launched cloud-based, AI-first platform in October 2024
- Voice-first solution with conversational AI
- Embedded agentic AI for smart assistance
- Real-time guideline deviation flagging
Revenue Cycle Management AI
XpertDox
- AI-powered medical coding with 94% automation rate
- 99% coding accuracy
- EHR-agnostic platform
- Nao Medical partnership results: 15% increase in charge capture, 60% improvement in quality code capture, 40% reduction in charge entry lag
Athelas
- AI-powered revenue cycle management
- Real-time insights into financial operations
- Claims processing to denials management automation
Interoperability and Data Exchange Solutions
Particle Health
- Record retrieval service interfacing with Epic and other EHRs
- Challenged Epic’s monopolistic practices in 2025 lawsuit
- Focus on value-based care data needs
Commure
- Ambient AI for scribing, note creation, coding, and ordering
- LLM-powered natural language EHR queries
- AI RCM for revenue workflow optimization
Challenges Facing AI Healthcare Solutions
Data Quality and Availability
- Training requires large, diverse, high-quality datasets
- Many small biotechs and healthcare organizations lack sufficient data
- Data silos prevent comprehensive model training
- Inconsistent data formats across systems
Integration Complexity
- Legacy system compatibility issues
- Real-time synchronization challenges cause data inconsistencies
- API limitations: downtime, rate limits, frequent updates
- Vendor-specific integration requirements
Interoperability Standards
- FHIR and HL7 adoption remains inconsistent
- Proprietary formats from major vendors
- Middleware solutions required to bridge old and new systems
Regulatory and Compliance Challenges
- HIPAA privacy requirements for AI systems
- FDA oversight for clinical decision support
- Liability concerns for AI-generated recommendations
- State-specific AI regulations emerging (e.g., Illinois ban on AI in mental healthcare)
Security Concerns
- AI models as potential attack vectors
- Data poisoning risks in federated systems
- Privacy preservation in model training
- Third-party AI service dependencies
Cost and ROI Uncertainty
- Significant upfront investment in AI infrastructure
- Licensing fees for AI tools
- Unclear long-term return on investment
- Ongoing maintenance and update costs
Clinical Validation Requirements
- Need for extensive testing before deployment
- Continuous monitoring for bias and errors
- Human oversight requirements
- Liability for AI-assisted decisions
The Incumbent Advantage
- Startups currently capture 85% of AI revenue among healthcare respondents
- However, customers prefer to buy AI from their incumbent EHR provider for most use cases
- Customers favor startups for ambient scribes and chart review
- EHR vendors preferred for coding, billing, prior authorization, scheduling, clinical decision support, and patient navigation
This creates a challenging landscape where innovative startups must compete against established EHR vendors who are rapidly building AI capabilities into their platforms.
Section 6: AI, LLMs, and Agentic AI as Solutions—Use Cases and ROI
Large Language Models (LLMs), Generative AI, and emerging Agentic AI represent a potential paradigm shift in addressing EHR challenges. These technologies can automate complex workflows, enhance clinical decision-making, and fundamentally reimagine how healthcare data serves both providers and patients.
Use Cases, ROI, and Patient Benefits
| Use Case | LLM/GenAI/Agentic AI Application | Provider ROI | Patient Benefit | Implementation Status |
|---|---|---|---|---|
| Clinical Documentation | Ambient listening converts conversations to structured notes | 50% reduction in documentation time 2+ hours saved per clinician per day $100K+ annual savings per physician 70% reduction in burnout |
More face-to-face time with providers Improved provider engagement Better care quality from focused attention |
Mature: 170+ organizations deployed, $600M market |
| Clinical Decision Support | LLM-powered diagnostic assistance and treatment recommendations | 20-30% reduction in diagnostic errors Faster treatment decisions Improved guideline adherence Reduced malpractice risk |
Earlier accurate diagnoses Personalized treatment plans Reduced adverse events Better outcomes |
Emerging: Epic 100+ AI functions, Oracle integration |
| Automated Medical Coding | AI extracts billable services from clinical notes | 94% automation of claims 99% coding accuracy 15% increase in charge capture 60% improvement in quality codes |
Faster insurance approvals Reduced billing errors Lower out-of-pocket costs |
Deployed: XpertDox, others operational |
| Prior Authorization | Agentic AI automates submission and follow-up | 40-50% reduction in time spent 80% faster approval times Reduced administrative staffing needs |
Faster access to care Fewer treatment delays Reduced care abandonment |
Pilot Stage: Payer integration ongoing |
| Patient Engagement | AI chatbots and virtual assistants | 30-40% reduction in call volume 24/7 patient support Reduced no-show rates |
Immediate answers Convenient scheduling Proactive health management |
Growing: Widely adopted |
| Medication Management | LLM analyzes interactions and contraindications | 50% reduction in adverse drug events Lower readmission rates Reduced liability |
Safer prescribing Personalized medication plans Improved adherence |
Operational: Built into EHRs |
| Population Health Management | Predictive models identify high-risk patients | 25-35% reduction in hospital admissions Lower costs via early intervention Improved value-based performance |
Proactive outreach Preventive care Better chronic disease management |
Mature: Widely deployed |
| Clinical Trial Matching | AI matches patients to trials | Faster recruitment Increased enrollment Research revenue |
Access to cutting-edge treatments Personalized options |
Emerging: TriNetX, others |
| Radiology Analysis | AI analyzes imaging for abnormalities | 30% faster read times Improved detection rates Standardized reporting |
Earlier detection Reduced false negatives Faster diagnoses |
Mature: FDA-cleared tools |
| Sepsis Prediction | Real-time monitoring with early warning | 20% reduction in mortality Shorter ICU stays Reduced treatment costs |
Lives saved Fewer ICU complications |
Operational: Epic Sepsis Model |
| Patient Education | Personalized education materials | Reduced patient calls Improved compliance Better outcomes |
Better understanding Improved self-care Reduced anxiety |
Growing: Portal integration |
| Care Coordination | AI identifies care gaps and coordinates referrals | 30% reduction in readmissions Improved metrics Enhanced transitions |
Comprehensive care Reduced duplicate testing Better outcomes |
Emerging: HIE integration |
| Voice Navigation of EHR | Natural language queries replace clicking | 40% reduction in time finding info Higher clinician satisfaction Reduced training time |
Faster responses More accurate sharing |
Early: Oracle voice-first EHR (2024) |
| Synthetic Data Generation | Creates realistic training data | Research acceleration Algorithm development Lower data acquisition costs |
Faster breakthroughs Personalized AI tools Privacy protection |
Emerging: Research use |
| Clinical Note Summarization | Summaries of lengthy records | 60% faster chart review Better handoffs Reduced cognitive load |
More informed providers Fewer gaps Better continuity |
Deployed: Epic summarization live |
Putting Patients at the Center with AI
The transformative potential of AI in healthcare lies in its ability to shift the focus from system efficiency to patient-centeredness:
Personalized Care at Scale
- AI can analyze individual patient data to recommend personalized treatment plans
- Genomic data integration enables precision medicine
- Social determinants of health factored into care planning
- Real-time adjustment of treatment based on patient response
Enhanced Patient Agency
- Natural language interfaces allow patients to query their own health data
- AI-powered chatbots provide 24/7 health guidance
- Personalized health education materials in patient’s preferred language
- Predictive models help patients understand their health trajectories
Proactive Rather Than Reactive Care
- Early warning systems prevent acute episodes
- Wearable integration enables continuous monitoring
- AI identifies patients who would benefit from preventive interventions
- Care gaps automatically flagged and addressed
Reduced Administrative Burden on Patients
- Automated scheduling and rescheduling
- Simplified insurance navigation
- Pre-visit data collection through conversational AI
- Post-visit follow-up and care plan reinforcement
The Data Quality Imperative
For AI to deliver on its promise, data quality is paramount. However, several factors complicate this:
Data Reliability Challenges
- Inconsistent data entry practices
- Copy-paste propagation of errors
- Outdated information persisting across systems
- Missing or incomplete data fields
- Unstructured data in free-text notes
The “Garbage In, Garbage Out” Problem
- AI models trained on biased or incomplete data perpetuate those biases
- Historical inequities in healthcare delivery embedded in training data
- Missing data from underserved populations limits model generalizability
- Algorithmic bias can worsen healthcare disparities
Solutions Emerging
- Data quality monitoring tools
- Standardized data collection protocols
- Automated data validation
- Human-in-the-loop verification for critical decisions
- Fairness and bias testing in AI model development
Section 7: The Privacy Paradox and Federated Learning
The promise of AI in healthcare faces a fundamental paradox: the most effective AI models require vast amounts of diverse data, yet privacy regulations and competitive interests prevent that data from being shared freely.
The Privacy and Data Sharing Challenge
PII and HIPAA Constraints Protected Health Information (PHI) and Personally Identifiable Information (PII) are subject to strict regulations:
- HIPAA regulations limit how patient data can be shared
- State privacy laws (CCPA, GDPR) add additional constraints
- De-identification requirements may reduce data utility
- Re-identification risks from sophisticated attacks
Competitive Barriers
- Healthcare organizations view patient data as competitive assets
- Sharing data with competitors is strategically unacceptable
- Pharmaceutical companies protect proprietary clinical trial data
- Fear of losing competitive advantage inhibits collaboration
The Centralized Data Model’s Limitations Traditional approaches to AI training require centralizing data:
- Security vulnerabilities from massive data repositories
- Single points of failure (as demonstrated by Change Healthcare breach)
- Regulatory approval challenges for data pooling
- Patient consent complications
Enter Federated Learning
Federated Learning offers a revolutionary approach: training AI models on distributed data without ever moving the data itself.
How Federated Learning Works
- Model Distribution: A central AI model is distributed to multiple locations (hospitals, clinics, research institutions)
- Local Training: Each location trains the model on its own local data, which never leaves the premises
- Update Aggregation: Only the model updates (learned patterns, not raw data) are sent back to the central server
- Model Improvement: The central server aggregates these updates to improve the global model
- Iteration: The improved model is redistributed, and the process repeats
Key Advantages
- Privacy preservation: Raw patient data never leaves the source
- Regulatory compliance: Meets HIPAA and other privacy requirements
- Reduced data transfer: Only model updates move across networks
- Diverse training: Models learn from heterogeneous populations
- Institutional autonomy: Organizations maintain control of their data
Eli Lilly TuneLab: A Groundbreaking Implementation
In September 2025, Eli Lilly launched TuneLab, one of the most ambitious federated learning platforms in healthcare, demonstrating the technology’s transformative potential.
The TuneLab Platform
Scale and Investment
- Built on $1+ billion of proprietary research data
- Trained on hundreds of thousands of unique molecules
- Represents decades of drug discovery expertise
- One of the industry’s most valuable AI datasets
Federated Architecture
- Powered by Rhino Federated Computing platform
- Uses NVIDIA FLARE for federated learning
- Third-party hosting ensures neutrality
- Partners share only model updates, never raw data
How It Works
- Biotech partners access Lilly’s AI models
- Partners fine-tune models on their own proprietary data
- Model improvements (not data) are shared back
- Continuous improvement benefits the entire ecosystem
- All parties maintain complete data privacy
Ecosystem Impact
- About a dozen startups joined initially, including Firefly Bio, Superluminal Medicines, Circle Pharma, and Insitro
- 16 ready-to-use models spanning discovery and preclinical workflows
- Predictive ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) models
- Cancer research data integration
- In vivo small molecule predictive models planned
The Competitive Advantage TuneLab represents a strategic shift:
- Smaller biotechs gain access to enterprise-scale AI capabilities
- Lilly benefits from diverse data improving their models
- Faster drug discovery across the industry
- Compressed decades of learning into accessible intelligence
Federated Learning in Healthcare EHR Ecosystem
The TuneLab model points toward how federated learning could transform the broken EHR ecosystem:
Multi-Institutional Clinical Research
- Hospitals could collaborate on AI model development without sharing patient data
- Rare disease research could leverage global patient populations
- Clinical trials could be designed with broader demographic representation
- Medical knowledge extracted from collective experience
Predictive Model Development
- Sepsis prediction models trained across diverse patient populations
- Readmission risk algorithms that account for regional variations
- Disease progression models incorporating socioeconomic factors
- Treatment response predictions personalized to local populations
Quality Improvement
- Benchmark clinical outcomes while preserving institutional privacy
- Identify best practices through pattern analysis
- Detect systemic issues across the healthcare system
- Continuous learning from clinical experience
Addressing Health Disparities
- Include underserved populations in model training without exploiting their data
- Develop AI that works equitably across demographics
- Identify and correct algorithmic bias
- Enable personalized medicine for all populations
Technical Challenges of Federated Learning
While promising, federated learning faces implementation hurdles:
Communication Overhead
- Frequent model updates require robust network infrastructure
- Bandwidth constraints in rural healthcare settings
- Latency in model convergence
Statistical Heterogeneity
- Non-IID (non-independent and identically distributed) data across sites
- Imbalanced datasets between large and small institutions
- Model performance may vary across different data distributions
System Heterogeneity
- Different computational capabilities at participating sites
- Varying software environments and EHR systems
- Synchronization challenges
Security Considerations
- Model updates can still leak information through sophisticated attacks
- Malicious participants could poison models
- Need for secure aggregation protocols
Governance and Incentives
- Who owns the resulting models?
- How are contributions valued and compensated?
- Ensuring equitable participation
- Managing intellectual property
Section 8: Real-World Examples of Healthcare Providers Using AI
Healthcare providers are moving beyond pilots to operationalize AI solutions that deliver measurable business and clinical benefits.
Cleveland Clinic: Comprehensive Ambient AI Deployment
Implementation Details
- Five-year partnership with Ambience Healthcare (announced February 2025)
- Deployed to over 4,000 caregivers
- Described as “one of the most successful technology launches” by the organization
Business Benefits
- Significantly reduced documentation burden
- Improved clinician satisfaction scores
- Enhanced ability to recruit and retain physicians
- Positioned as innovation leader
Clinical Outcomes
- More time for patient interaction
- Improved care quality from better provider engagement
- Better work-life balance for clinicians
Lessons Learned
- Careful pilot site selection critical
- Partnership approach with early-stage companies valuable
- Deployment into practice is the true test of AI viability
Kaiser Permanente: AI Scribe Implementation
Implementation Scale
- AI scribe technology deployed across multiple facilities
- Supporting thousands of patient encounters daily
Documented Results
- Clinicians save up to 2 hours per day on documentation
- Patient satisfaction scores exceed 92%
- Reduced clinician burnout reported
- Improved access as physicians can see more patients
Business Impact
- Significant productivity gains
- Improved clinician retention
- Enhanced patient experience scores
- Positive ROI within first year
Houston Methodist: Smart Hospital Initiative
Comprehensive Technology Integration
- Over 11 million square feet covered by RTLS (Real-Time Location Services)
- Cameras in all patient rooms, emergency rooms, and ORs
- Wearable vital sign monitors for continuous patient monitoring
- Ambient voice technology for documentation
AI Applications
- Hospital bed alerts before patient distress
- Continuous vital sign monitoring
- Camera systems for remote clinician collaboration
- Smart concierge for appointment scheduling and patient calls
Business Benefits
- Thousands of hours returned to bedside nursing
- Reduced clinician burnout
- Improved operational efficiency
- Enhanced patient safety
Future Plans
- Moving away from clerical data entry entirely
- Drone delivery for critical medicines
- Self-service scheduling and payment
- AI-based support for patients and staff
Tampa General Hospital and Health Systems
AI Strategy
- Deploying ambient AI for clinical documentation
- Focus on workflow integration
- Emphasis on clinician experience
Implementation Approach
- Intentional about pilot site selection
- Good partnership with AI companies
- Staged rollout based on learnings
Northeast Medical Specialists (NEMS)
Challenge
- Language barriers with diverse patient population
- High documentation burden
- Provider burnout
Solution
- Commure’s Epic-integrated Ambient AI
- Multilingual support
Results
- Near-perfect note accuracy
- 30% reduction in documentation time
- Improved patient communication
- Better provider satisfaction
Dignity Health Dr. Palakurthy (Internal Medicine)
Implementation
- Commure AI scribe technology
- Solo practitioner setting
Time Savings
- Up to 3 hours saved per day on charting
- 4 additional hours saved each weekend
- More time for patient messages and prescriptions
Business Impact
- Able to maintain patient volume with less stress
- Improved work-life balance
- Enhanced quality of patient interactions
- More sustainable practice model
Mount Sinai Health: Digital Navigation
Program Design
- Partnership with Commure Engage
- Comprehensive digital navigation for joint replacement patients
- Three therapeutic modules for surgical preparation and recovery
Integration
- Prescribable via EHR
- Guides patients and caregivers through entire care journey
- Pre-visit and post-visit patient interviews
Outcomes
- Better patient preparation for surgery
- Improved recovery outcomes
- Reduced complications
- Higher patient satisfaction
Nao Medical: AI-Powered Revenue Cycle Management
Challenge
- Integration issues affecting charge capture
- Inconsistent coding quality
- Delayed charge entry
Solution
- XpertDox AI coding platform
- Automated coding with NLP
- EHR-agnostic integration
Quantifiable Results
- 15% increase in charge capture
- 60% improvement in quality code capture
- 40% reduction in charge entry lag
- Significant revenue impact
Common Success Factors Across Implementations
Strategic Approach
- Clear definition of problems to solve
- Stakeholder engagement from the beginning
- Realistic expectations and timelines
- Measurement frameworks in place
Technology Selection
- Careful vendor evaluation
- Proof-of-concept before full deployment
- Integration capabilities with existing systems
- Scalability considerations
Change Management
- Comprehensive training programs
- Ongoing support and optimization
- Physician champions driving adoption
- Iterative refinement based on feedback
Business Case
- Clear ROI metrics defined upfront
- Combination of hard and soft benefits
- Time horizon for payback realistic
- Ongoing value capture measured
Section 9: The Future—Policy Changes, AI’s Role, and Business Growth
The healthcare landscape is undergoing seismic shifts driven by policy changes, economic pressures, and technological transformation. Understanding these dynamics is critical for healthcare enterprises seeking to thrive in the coming decade.
The Changing Policy Landscape
Medicaid Reforms and Implications While specific 2025 Medicaid cuts are still being debated in Congress, broader trends are clear:
- Shift toward managed care models
- Increased emphasis on value-based reimbursement
- Stricter eligibility requirements in many states
- Potential reduction in federal matching funds
Impact on American Patients
- Reduced access to care for vulnerable populations
- Increased uncompensated care burden on safety-net providers
- Healthcare deserts expanding in rural and underserved areas
- Growing disparities in health outcomes
Global Healthcare Policy Trends
- Universal healthcare systems facing sustainability challenges
- Aging populations straining healthcare budgets
- Shift from volume to value globally
- Digital health integration accelerating worldwide
AI as the Bridge Between Quality and Economics
Cost Containment Without Compromising Care AI offers a path to reduce costs while maintaining or improving quality:
Administrative Automation
- Prior authorization automation reduces delays and staffing needs
- Automated coding and billing reduces revenue cycle costs
- Intelligent scheduling optimizes resource utilization
- Supply chain optimization reduces waste
Clinical Efficiency
- Ambient documentation reduces physician time burden
- Clinical decision support reduces unnecessary testing
- Predictive analytics prevents costly complications
- Care coordination AI reduces readmissions
Population Health Management
- Identify high-risk patients before acute episodes
- Personalize preventive care interventions
- Optimize chronic disease management
- Address social determinants of health systematically
Estimated Savings Potential Healthcare economists project AI could reduce U.S. healthcare spending by:
- Administrative costs: 20-30% reduction ($120-180B annually)
- Clinical inefficiencies: 10-15% reduction ($200-300B annually)
- Preventable complications: 15-25% reduction ($150-250B annually)
- Total potential: $470-730 billion in annual savings by 2030
Enterprise Profitability Through AI
Revenue Enhancement
- Improved charge capture through AI coding (15%+ improvement)
- Reduced denials through intelligent claims submission
- New revenue streams from virtual care
- Participation in value-based contracts enabled by analytics
Cost Reduction
- Reduced staffing needs for administrative tasks
- Lower malpractice costs from clinical decision support
- Reduced readmissions and complications
- Optimized workforce scheduling
Competitive Differentiation
- Attract and retain top clinical talent with better work environment
- Market position as innovation leader
- Higher patient satisfaction scores
- Better quality metrics for contracting
Patient Acquisition and Retention
- Enhanced patient experience through AI
- Better outcomes drive referrals
- Convenience factors (AI scheduling, virtual care)
- Personalized engagement increases loyalty
AI for Serving Patients and Growing the Business
The Virtuous Cycle
- Better Patient Experience → Improved satisfaction scores and retention
- Reduced Clinician Burden → Better recruitment and retention of talent
- Improved Outcomes → Higher quality scores and value-based payments
- Data-Driven Insights → Continuous improvement and innovation
- Operational Efficiency → Resources freed for strategic initiatives
- Market Differentiation → Growth in patient volume and market share
Strategic Imperatives for Healthcare Enterprises
1. Build AI-Ready Infrastructure
- Invest in cloud-based, interoperable EHR platforms
- Establish data governance frameworks
- Create data lakes with clean, standardized data
- Implement robust cybersecurity
2. Develop AI Capabilities Organizationally
- Create AI governance committees
- Hire or develop AI expertise
- Establish partnerships with AI vendors
- Build internal AI development capacity
3. Focus on High-Impact Use Cases
- Start with areas of greatest pain (documentation burden)
- Expand to clinical decision support
- Scale to population health management
- Eventually pursue predictive and preventive capabilities
4. Prioritize Clinician Experience
- Involve frontline staff in technology selection
- Provide comprehensive training and support
- Measure and optimize usability
- Create feedback loops for continuous improvement
5. Emphasize Patient-Centricity
- Deploy AI that enhances patient experience
- Ensure equity in AI deployment
- Maintain human touch in care delivery
- Transparent communication about AI use
6. Build Data Partnerships
- Participate in federated learning networks
- Collaborate on AI model development
- Share de-identified data for research
- Contribute to industry-wide improvement
The Global Perspective
International AI Healthcare Adoption
Countries are taking different approaches to healthcare AI:
United Kingdom
- 87% of clinicians using EHRs frequently
- £200+ million annually in digital health investment
- NHS AI Lab driving innovation
- 60% of NHS hospitals using shared EHR systems
Canada
- 500,000 potential EHR users among healthcare professionals
- National digital health strategy
- Focus on interoperability across provinces
Australia
- 90%+ of general practices using EHRs
- My Health Record national platform
- AUD 2+ billion in digital health investments
Germany
- 80% of GPs using EHR systems
- 70% of hospitals with EHRs
- 53% of providers exchanging data electronically
Lessons for the U.S.
- Universal platforms enable better data sharing
- Government coordination accelerates adoption
- National digital strategies provide direction
- Public investment critical for equitable access
The 2030 Vision: AI-Powered, Patient-Centered Healthcare
What Success Looks Like By 2030, if current trajectories continue:
For Patients:
- Seamless care experiences across all providers
- Real-time access to all health information
- AI-powered health coaching and guidance
- Predictive alerts preventing health crises
- Personalized treatment plans based on individual biology
- Reduced healthcare costs from better efficiency
For Providers:
- Documentation burden largely eliminated
- AI assistants handling routine tasks
- More time for complex decision-making and patient interaction
- Work-life balance restored
- Professional satisfaction improved
- Reduced burnout and turnover
For Healthcare Enterprises:
- 30-40% reduction in administrative costs
- 15-25% improvement in clinical outcomes
- Higher patient satisfaction and loyalty
- Sustainable profitability even with constrained reimbursement
- Market leadership through innovation
- Contributions to population health improvement
For the Healthcare System:
- $500+ billion in annual cost savings
- Improved health equity through targeted interventions
- Faster medical breakthroughs through data collaboration
- Resilient infrastructure for future challenges
- Global leadership in healthcare innovation
Section 10: Conclusion—Technology, Business, and Patients
The evolution of Electronic Health Records in America tells a story of ambitious promises, hard-won progress, and persistent challenges. From the dark days of paper charts and illegible handwriting to today’s sophisticated digital ecosystems, we have come far. Yet the journey is far from complete.
Summarizing the Journey
Where We’ve Been
- The HITECH Act catalyzed a revolution in healthcare IT, driving adoption from 3% to over 85% in less than a decade
- Billions of dollars invested in digital infrastructure
- Near-universal EHR adoption achieved among hospitals and physicians
- Meaningful use evolved into promoting interoperability
Where We Are
- A broken system characterized by poor interoperability
- Monopolistic dynamics limiting competition and innovation
- Healthcare providers suffering from unprecedented burnout
- Patients experiencing fragmented care despite digital records
- AI solutions emerging but facing integration and adoption challenges
- Regulatory complexity creating barriers and confusion
The Promise of Transformation Artificial intelligence, particularly through innovative approaches like federated learning, offers genuine hope for transforming healthcare delivery:
For Technology:
- AI can finally deliver on the promise of interoperability by understanding and translating between systems
- Federated learning enables collaboration without data sharing, preserving privacy and competitive interests
- Agentic AI can handle complex workflows autonomously
- Natural language interfaces can make systems intuitive
- Continuous learning from collective experience drives improvement
For Business:
- Administrative automation reduces costs by 20–30%
- Improved clinical efficiency saves hundreds of billions
- Better outcomes drive value-based payment success
- Enhanced patient and clinician experience creates competitive advantage
- Sustainable profitability even with constrained reimbursement
- Market differentiation through innovation leadership
For Patients:
- More face-to-face time with engaged, attentive providers
- Seamless care coordination across all settings
- Proactive rather than reactive healthcare
- Personalized treatment based on individual biology
- Reduced costs from improved efficiency
- Better outcomes from earlier intervention
- Enhanced safety from clinical decision support
- Greater agency over their own health through accessible information
The Challenges Ahead
Success is not guaranteed. Significant obstacles remain:
Technical Challenges
- Achieving true interoperability across legacy systems
- Ensuring AI model safety and reliability
- Addressing algorithmic bias and health equity
- Managing the complexity of federated learning at scale
- Protecting privacy while enabling data utilization
Economic Challenges
- Justifying upfront AI investment
- Navigating uncertain regulatory landscape
- Managing change across large organizations
- Competing against incumbent EHR monopolies
- Ensuring equitable access to AI benefits
Human Challenges
- Overcoming clinician skepticism and change fatigue
- Maintaining human judgment in AI-augmented care
- Addressing workforce displacement concerns
- Building trust in AI systems
- Preserving the human connection in healthcare
Policy Challenges
- Evolving regulations to enable innovation while ensuring safety
- Addressing reimbursement for AI-enabled care
- Managing liability for AI-assisted decisions
- Ensuring equitable access to AI benefits
- Balancing innovation with patient protection
The Path Forward
Success requires coordinated action across the ecosystem:
For Healthcare Providers:
- Invest strategically in AI infrastructure and capabilities
- Prioritize clinician experience in technology decisions
- Start with high-impact use cases and scale iteratively
- Measure outcomes rigorously and optimize continuously
- Participate in data collaboration through federated learning
For Technology Vendors:
- Build truly interoperable systems using open standards
- Design for clinician experience, not just feature lists
- Partner transparently with healthcare organizations
- Invest in safety, reliability, and bias mitigation
- Enable rather than obstruct data sharing
For Policymakers:
- Update regulations to enable innovation while protecting patients
- Incentivize data sharing through federated learning
- Address market concentration and anti-competitive practices
- Support digital infrastructure in underserved areas
- Fund research on AI in healthcare
For Patients:
- Engage with digital health tools
- Provide feedback on technology experiences
- Advocate for better interoperability
- Participate in data sharing for research when comfortable
- Hold providers and payers accountable for AI equity
The Ultimate Vision
Healthcare is fundamentally about human connection—the sacred relationship between healer and patient. Technology should amplify that connection, not diminish it. AI and federated learning offer a path to realize this vision:
Imagine a future where:
- Physicians look into patients’ eyes, not at computer screens
- Critical health information flows seamlessly wherever needed
- Diseases are predicted and prevented before symptoms appear
- Every patient receives care personalized to their unique biology
- Healthcare costs decline while quality improves
- Health equity is achieved through targeted, data-driven interventions
- Medical breakthroughs accelerate through global data collaboration
- The burden of administration lifts, allowing caregivers to focus on caring
This future is achievable, but it requires commitment, investment, and collaboration. The technology exists. The business case is compelling. The patient need is urgent. What remains is the will to transform a broken system into one that truly serves human flourishing.
The evolution of EHR in America is not complete. We stand at an inflection point where the next decade could see either continued frustration with marginal improvements, or genuine transformation that fulfills the original promise of digital healthcare. The choice is ours.
Section 11: References and Resources
Market Research and Statistics
- Grand View Research. (2024). “U.S. Electronic Health Records Market Report, 2030.” https://www.grandviewresearch.com/industry-analysis/us-electronic-health-records-market-report
- Technavio. (2025). “Electronic Health Records Market Growth Analysis – Size and Forecast 2025-2029.” https://www.technavio.com/report/electronic-health-records-market-industry-analysis
- Roots Analysis. (2025). “Electronic Health Records Market Size, Share, Trends Report [2035].” https://www.rootsanalysis.com/reports/electronic-health-records-market.html
- Precedence Research. (2025). “Electronic Health Records Market Size to Hit USD 44.39 Bn by 2034.” https://www.precedenceresearch.com/electronic-health-records-market
- Market.us Media. (2025). “EHR Industry Statistics and Facts (2025).” https://media.market.us/ehr-industry-statistics/
- Mordor Intelligence. (2025). “Electronic Medical Records Market Size, Report, Share & Growth Trends 2030.” https://www.mordorintelligence.com/industry-reports/global-electronic-medical-records-market-industry
- KLAS Research. (2025). “US Acute Care EHR Market Share 2025.” https://klasresearch.com/report/us-acute-care-ehr-market-share-2025
- Mordor Intelligence. (2025). “Ambulatory EHR Market Size | Analysis Report 2025-2030.” https://www.mordorintelligence.com/industry-reports/ambulatory-ehr-market
- Mordor Intelligence. (2025). “Clinical EHR Systems Market Size, Growth and Forecast | Industry Analysis 2030.” https://www.mordorintelligence.com/industry-reports/clinical-ehr-market
HITECH Act and Policy
- HIPAA Journal. (2025). “What is the HITECH Act? 2025 Update.” https://www.hipaajournal.com/what-is-the-hitech-act/
- Wikipedia. (2025). “Health Information Technology for Economic and Clinical Health Act.” https://en.wikipedia.org/wiki/Health_Information_Technology_for_Economic_and_Clinical_Health_Act
- Blumenthal, D., & Tavenner, M. (2010). “The ‘Meaningful Use’ Regulation for Electronic Health Records.” NEJM.
- Adler-Milstein, J., et al. (2015). “Electronic Health Record Adoption in US Hospitals.” Health Affairs.
- PMC. “Assessing HITECH Implementation and Lessons: 5 Years Later.” https://pmc.ncbi.nlm.nih.gov/articles/PMC5020152/
- Sprypt. (2025). “When did the Mandate for Electronic Health Records Begin?” https://www.sprypt.com/blog/are-emr-obligated-to-provide-care
- CMS. “CMS AND ONC FINAL REGULATIONS DEFINE MEANINGFUL USE.” https://www.cms.gov/newsroom/fact-sheets/cms-and-onc-final-regulations-define-meaningful-use-and-set-standards-electronic-health-record
- Caseguard. (2024). “The HITECH Act and the Implementation of EHR, Privacy.” https://caseguard.com/articles/the-hitech-act-and-the-implementation-of-electronic-health-records/
- AMA Journal of Ethics. (2011). “THE HITECH ACT: An Overview.” https://journalofethics.ama-assn.org/article/hitech-act-overview/2011-03
- Strategic Management Services. (2025). “An Overview of HITECH Act Incentives & Regulations.” https://www.compliance.com/resources/hitech-act-update-an-overview-of-the-medicare-and-medicaid-ehr-incentive-programs-regulations/
- Particle Health. (2022). “Meaningful Use and the HITECH Act.” https://www.particlehealth.com/blog/hitech-act-meaningful-use
- Sprypt. (2025). “Charting EHR History: Evolution Through Innovation.” https://www.sprypt.com/blog/emr-history
EHR Challenges and Interoperability
- Medical Economics. (2025). “Epic EHR monopoly violates federal antitrust laws…” https://www.medicaleconomics.com/view/epic-ehr-monopoly…
- Dash Technologies. (2025). “Epic EHR Integration Challenges.” https://dashtechinc.com/blog/overcoming-common-challenges-in-epic-ehr…
- Dash Technologies. (2025). “Epic vs Other EHR Integration Systems.” https://dashtechinc.com/blog/epic-ehr-integration-vs-other-systems…
- 4sight Health. (2022). “Healthcare’s Epic Problem.” https://www.4sighthealth.com/healthcares-epic-problem…
- HealthTECH Resources. (2025). “Epic Consultant Insights.” https://healthtechresourcesinc.com/epic-consultant-insights…
- Becker’s Hospital Review. (2025). “‘Big Bang’ Epic Go-Lives.” https://www.beckershospitalreview.com/…big-bang-epic-go-lives
- Vsoft Consulting. (2025). “5 Complaints About EPIC Systems.” https://blog.vsoftconsulting.com/blog/5-complaints-about-epic-systems
- TechTarget. “Particle Health sues Epic Systems.” https://www.techtarget.com/…/Particle-Health-sues-Epic
- Wikipedia. (2025). “Epic Systems.” https://en.wikipedia.org/wiki/Epic_Systems
- Becker’s Hospital Review. (2023). “Why Epic Opposes New Interoperability Rules.” https://www.beckershospitalreview.com/…interoperability…
Physician Burnout and EHR Impact
- PMC. “Burnout Related to Electronic Health Record Use in Primary Care.” Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10134123/
- AHRQ. “Physician Burnout | Agency for Healthcare Research and Quality.” Available at: https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html
- PMC. “Physician Burnout and the Electronic Health Record Leading Up to and During the First Year of COVID-19: Systematic Review.” Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9015762/
- AAFP. (2019). “Study: EHRs Contribute to Family Physician Stress, Burnout.” Available at: https://www.aafp.org/news/practice-professional-issues/20190116ehrstudy.html
- Oxford Academic. (2023). “Association of physician burnout with perceived EHR work stress and potentially actionable factors.” Journal of the American Medical Informatics Association. Available at: https://academic.oup.com/jamia/article/30/10/1665/7227290
- AMA. (2020). “7 things about EHRs that stress out doctors.” Available at: https://www.ama-assn.org/practice-management/digital/7-things-about-ehrs-stress-out-doctors
- Health Catalyst. “Physician Burnout and the EHR: Addressing Five Common Burdens.” Available at: https://www.healthcatalyst.com/learn/insights/physician-burnout-ehr-addressing-5-top-burdens
- JMIR Medical Informatics. (2024). “Evaluating the Prevalence of Burnout Among Health Care Professionals Related to Electronic Health Record Use: Systematic Review and Meta-Analysis.” Available at: https://medinform.jmir.org/2024/1/e54811
- PMC. “Physician Burnout: Evidence-Based Roadmaps to Prioritizing and Supporting Personal Wellbeing.” Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10773242/
- Mayo Clinic Proceedings. (2024). “Predicting Primary Care Physician Burnout From Electronic Health Record Use Measures.” Available at: https://www.mayoclinicproceedings.org/article/S0025-6196(24)00037-5/fulltext
AI Solutions in Healthcare
- Menlo Ventures. (2025). “2025: The State of AI in Healthcare.” Available at:
- The Healthcare Technology Report. (2025). “The Top 25 Healthcare AI Companies of 2025.” Available at:
https://thehealthcaretechnologyreport.com/the-top-25-healthcare-ai-companies-of-2025/
- Microsoft Industry Blogs. (2025). “A new era of ambient intelligence in healthcare.” Available at:
- SPSoft. (2025). “Epic EHR AI Trends For 2025: Reshaping Healthcare With GenAI.” Available at:
Epic EHR AI Trends for 2025: Reshaping Healthcare with GenAI Integration
- TechTarget. “How ambient AI fixed the EHR’s patient experience problems.” Available at:
https://www.techtarget.com/patientengagement/feature/How-ambient-AI-fixed-the-EHRs-patient-experience-problems
- Healthcare IT News. “AI Roundup: Ambient recording for emergencies and more EHR enhancements.” Available at:
https://www.healthcareitnews.com/news/ai-roundup-ambient-recording-emergencies-and-more-ehr-enhancements
- Fierce Healthcare. (2025). “Oracle Health debuts AI-powered EHR designed as a ‘voice-first’ solution embedded with agentic AI.” Available at:
https://www.fiercehealthcare.com/health-tech/oracle-health-debuts-ai-powered-ehr-designed-voice-first-solution-embedded-agentic-ai
- The Healthcare Technology Report. (2025). “The Top 25 Healthcare Software Companies of 2025.” Available at:
https://thehealthcaretechnologyreport.com/the-top-25-healthcare-software-companies-of-2025/
- Commure. “AI Solutions Co-Developed with Health Systems.” Available at:
https://www.commure.com/
- Fierce Healthcare. (2025). “Healthcare players refine their AI and tech strategies: Key trends and takeaways from HLTH 2025.” Available at:
https://www.fiercehealthcare.com/health-tech/key-trends-and-executive-takeaways-hlth-2025
Federated Learning and Eli Lilly TuneLab
- Eli Lilly Investor Relations. (2025). “Lilly launches TuneLab platform to give biotechnology companies access to AI-enabled drug discovery models.” Available at:https://investor.lilly.com/news-releases/news-release-details/lilly-launches-tunelab-platform-give-biotechnology-companies
- Drug Discovery Trends. (2025). “Eli Lilly launches TuneLab to share AI drug discovery models with biotechs.” Available at:
Lilly launches TuneLab, sharing AI drug-discovery models with biotechs
- CNBC. (2025). “Eli Lilly, Nvidia partner to build supercomputer, AI factory for drug discovery and development.” Available at: https://www.cnbc.com/2025/10/28/eli-lilly-nvidia-supercomputer-ai-factory-drug-discovery.html
- PR Newswire. (2025). “Lilly partners with NVIDIA to build the industry’s most powerful AI supercomputer.” Available at:https://www.prnewswire.com/news-releases/lilly-partners-with-nvidia-to-build-the-industrys-most-powerful-ai-supercomputer-supercharging-medicine-discovery-and-delivery-for-patients-302597285.html
- BioPharma Dive. (2025). “Lilly to give biotech startups access to AI tools.” Available at: https://www.biopharmadive.com/news/eli-lilly-biotech-ai-tunelab-drug-discovery-startups/759630/
- NVIDIA Blog. (2025). “Lilly Deploys World’s Largest, Most Powerful AI Factory for Drug Discovery Using NVIDIA Blackwell-Based DGX SuperPOD.” Available at: https://blogs.nvidia.com/blog/lilly-ai-factory-nvidia-blackwell-dgx-superpod/
- Fierce Biotech. (2025). “Eli Lilly invites biotechs to use its new AI platform to help develop their own drugs.” Available at: https://www.fiercebiotech.com/biotech/lilly-invites-biotechs-use-its-new-ai-platform-help-develop-their-drugs
- PharmExec. (2025). “Lilly Forms Partnership with NVIDIA to Create AI Supercomputer.” Available at:https://www.pharmexec.com/view/lilly-forms-partnership-nvidia-create-ai-supercomputer
- Eli Lilly Investor Relations. (2025). “Lilly partners with NVIDIA to build the industry’s most powerful AI supercomputer.” Available at:https://investor.lilly.com/news-releases/news-release-details/lilly-partners-nvidia-build-industrys-most-powerful-ai
- VOH Network. (2025). “Eli Lilly Launches AI-Powered Lilly TuneLab for Biotech Innovation.” Available at:https://vohnetwork.com/news/healthtech/eli-lilly-launches-ai-powered-lilly-tunelab-for-biotech-innovation